Dr. Joel Salinas, MD, MBA, MSc, FAAN
Neurologist, Researcher, Author & Founder of Isaac Health

About me
As a college student, I traveled to the Amazon rainforest in Brazil to investigate mercury contamination in a local watershed. I asked affected villagers to share their experiences while I was there, and I learned something that has stayed with me since.
Decades prior, public health authorities warned the locals not to drink the water or eat the fish because of the risk of mercury poisoning. The majority of the villagers, however, disregarded these warnings until, one day, the warning came from their village’s shaman, a person they deeply trusted. Unlike the public health officials, the shaman listened to the persons he cared for with an extraordinary level of empathy, compassion, and kindness. This experience transformed the way I view health and society and strengthened my resolve to pursue a career in medicine.
During medical school, I learned about the fascinating ways in which our nervous system is the center of our thoughts, emotions, and actions; it is at the core of what makes each of us who we are. It became undeniable — my calling was neurology.
I chose to specialize in behavioral neurology because I saw in it a vision, a way to make a difference in the lives of everyone. This subspecialty of neurology provided me with additional training to better assist patients with extremely common but incurable brain disorders
Now, more than two decades later, at Isaac Health, we treat persons with neurodegenerative diseases that cause cognitive decline and impairment. These conditions, which arise when nerve cells lose function and perish, include Alzheimer’s disease, the most prevalent cause of dementia in elderly individuals. Other disorders we treat include the most common cause of dementia in adults under the age of 65, frontotemporal degeneration which involves the death of nerve cells in parts of the brain behind the forehead or ears. In addition to Parkinson’s disease and Lewy body dementia, we also manage vascular dementia, which results from an obstruction or reduction in blood flow to the brain.
The foundation of our treatment strategy is evidence-based. We prescribe medication when necessary, weighing risks and benefits, and refer patients to other specialists. These professionals include psychiatrists, neuropsychologists, cognitive, occupational, and physical therapists, as well as speech therapists. When appropriate, we offer patients access to new disease-modifying treatment and access to research studies and clinical trials.
We also recommend lifestyle and behavioral changes, such as exercise, a brain-healthy diet, and cognitively stimulating activities. Our recommendations include ways to lower stress and get help for anxiety, depression, post-traumatic stress disorder, and other mental health struggles.
We also connect patients, their families, and other caregivers to vital support services. We provide assistance with counseling, support, education, resource access, and care planning.
We strive to provide the best in compassionate and comprehensive care. We talk about different treatment choices and possible outcomes. We are honest and upfront about the many unknowns that often come with brain conditions.
We take pride in making a difference in people’s lives and making even the hardest situations a little bit easier to manage. Many of our patients say that we are very attentive, warm, knowledgeable, and genuinely care about them.
My National Institutes of Health-funded research focuses on the effect of psychosocial factors on mental health. For instance, I am investigating the influence of social isolation and loneliness as dementia risk factors. My objective is to help develop novel strategies that effectively reduce the risk of cognitive decline and dementia.
I am the author of Mirror Touch: A Memoir of Synesthesia and the Hidden Brain. To learn about this and more, you can listen to a recent episode of the NYU Langone Health and SiriusXM podcast Vital Signs or visit joelsalinasmd.com.
Credentials
Positions
Chief Medical Officer, Isaac Health
Clinical Associate Professor, Department of Neurology at NYU Grossman School of Medicine
Brain Health Initiative Member, Brain Health Committee, American Academy of Neurology
Editorial Board, Brain & Life magazine
Board Certifications
American Board of Psychiatry & Neurology - Neurology, 2015
United Council of Neurologic Subspecialties - Behavioral Neurology & Neuropsychiatry, 2016
Education
MSc in Epidemiology from the Harvard TH Chan School of Public Health, 2016
MD with Distinction from the University of Miami Miller School of Medicine, 2011
MBA with Distinction in All Subjects from the University of Miami Herbert Business School, 2011
BA with Distinction in All Subjects from Cornell University, 2005
Training
Research Fellow, Massachusetts General Hospital, Robert Katzman Clinical Research Training Fellowship in Alzheimer’s and Dementia Research from the American Academy of Neurology, American Brain Foundation, and the Alzheimer’s Association, 2018
Research Fellow, Harvard TH Chan School of Public Health, Neurostatistics and Neuroepidemiology T32 Fellowship, 2018
Clinical Fellow, Massachusetts General Hospital, Behavioral Neurology, 2016
Research Fellow, Massachusetts General Hospital, Schwamm-Marriott Clinical Care Research Fellowship, 2016
Chief Resident, Mass General Brigham, Neurology, 2015
Resident with Distinctions in Medical Education, Basic Science, Translational & Clinical Investigation, and Patient Safety, Quality Care & Health Policy, Mass General Brigham, Neurology, 2015
Intern, Massachusetts General Hospital, Internal Medicine, 2009
Research Fellow, University of Iowa Carver College of Medicine, Doris Duke Clinical Research Program, 2009
Research
As a behavioral neurologist with expertise in epidemiology and health outcomes research, my research goal has been to figure out how our social environments and brain biology are connected. We can then use what we learn to come up with and implement interventions that are universal, precise, and centered on people to improve brain health at the population level.
For our society to do well, we need brains that work well. Yet dementia and cerebrovascular disease continue to be incredibly prevalent and debilitating neurologic diseases; most drug trials to treat Alzheimer's disease and other causes of dementia have historically been unsuccessful. Thus, these age-related neurologic disorders are not just a looming threat to our society, but an ongoing threat to each of us and our loved ones.
Many known risk factors for these diseases are based in biology and physiology, like genetics and high blood pressure. However, a growing body of evidence suggests that a group of potentially changeable risk factors called "psychosocial determinants" may have a big impact on the risk and course of these diseases much further upstream. One psychosocial factor that is of particular interest is social ties. Stronger social ties, which include both functional parts (social support) and structural parts (social networks), are linked to better physical and mental health. Evidence linking social isolation and loneliness to a higher risk of stroke, cognitive dysfunction, and the buildup of Alzheimer's disease pathology suggests that a socially-based approach to possible therapeutic targets is needed....
If we look at how psychosocial factors affect brain health, we could learn how to use them for protection and treatment. Underlying molecular responses to genetic and environmental exposures start early in the development of disease. This makes it possible to find neurobiological pathways for the psychosocial determinants of brain health by studying related preclinical molecular, physiological, neuropsychological, and imaging markers of cognitive decline. As a result, this work leverages the interaction of biology and sociology to understand the mechanisms by which social settings change brain biology and then applies these discoveries to promote population brain health. In particular, my research uses socio-behavioral science, health outcomes research methods, and mathematical network theory in longitudinal epidemiologic cohorts to find out how a person’s social environment affects brain health outcomes, especially cognitive resilience and markers of vulnerability for cognitive decline. Based on these findings, psychosocial interventions are then made to strike a balance between being universal (able to be scaled at the population level; equally representative of and accessible to underrepresented minority groups) and precise (despite being universal, the same intervention is made to be complex and nuanced enough on the “back end” that it can dynamically address specific barriers, motivations, needs, and other characteristics at the level of the individual), and human-centered (committed to authentic empathy, compassion, and kindness, involving the human perspective in all steps of the process with a focus on improving brain health outcomes that truly matter to each person). This research approach is uniquely positioned to contribute to the next generation of insights, tools, and strategies that will ultimately: (1) provide practical and empowering guidance to patients, clinicians, and caregivers; (2) clarify the temporal relationship between dynamic social determinants in relation to risk and biological progression of cognitive decline; (3) improve intervention studies in Alzheimer’s disease and related conditions; and (4) extend beyond neurology to improve our broader understanding of psychosocial determinants of health and aging.
By learning more about the psychosocial factors that affect brain health, we will be able to create a new, paradigm-shifting clinical approach to treat neurologic diseases that come with age and drastically improve health at the population level. At the very least, this work will lead to useful results that can be used to put other work into context, help plan future health interventions, and support new areas of clinical study in neurology. Long-term, the goal of this work is to improve these methods and approaches so that they can be used to create a virtuous cycle between the physical, mental, and social parts of health that are needed for all of us to thrive.
Highlighted Publications
Association Of Loneliness With 10-Year Dementia Risk And Early Markers Of Vulnerability For Neurocognitive Decline
Salinas, Joel; Beiser, Alexa S; Samra, Jasmeet K; O’Donnell, Adrienne; DeCarli, Charles S; Gonzales, Mitzi M; Aparicio, Hugo J; Seshadri, Sudha
Neurology. 2022 Mar 29; 98(13):e1337-e1348
Salinas, Joel; O’Donnell, Adrienne; Kojis, Daniel J; Pase, Matthew P; DeCarli, Charles; Rentz, Dorene M; Berkman, Lisa F; Beiser, Alexa; Seshadri, Sudha
JAMA Network Open. 2021 Aug 02; 4(8):e2121122
Related News
Understanding FTD: What You Need to Know About the Most Common Dementia Under 60, Its Causes, Symptoms, and Treatment Options, in Light of Bruce Willis’ Diagnosis
As a behavioral neurologist and researcher at NYU Langone Health and

Life’s Simple 8: How These Habits Can Reduce Your Risk of Dementia
Discover how simple lifestyle changes can reduce your risk of dementia.
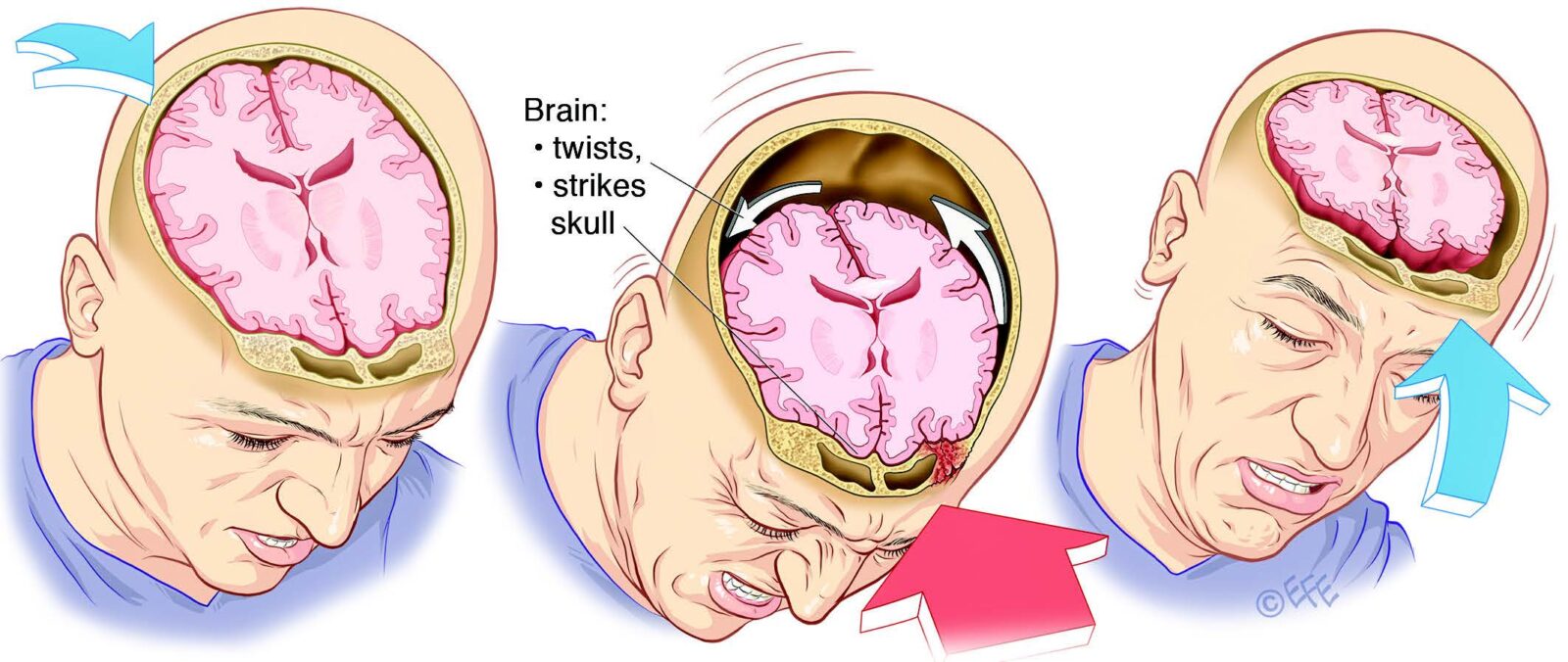
What You Need to Know About Concussion
In recent news, Senate Minority Leader Mitch McConnell suffered a concussion




