Introduction: On July 6, 2023, the FDA granted full approval to Lecanemab (Leqembi), marking a significant milestone as the first disease-modifying treatment for Alzheimer’s disease to receive such approval. This white paper aims to inform health insurance employees about the implications of Leqembi’s approval and offer insights into coverage considerations and potential cost implications.
Coverage Announcement by Centers for Medicare & Medicaid Services (CMS): The Centers for Medicare & Medicaid Services (CMS) have announced the coverage of Leqembi through Medicare. However, this coverage is contingent upon the collection of patient data as part of a disease registry. CMS has taken steps to remove barriers by establishing the Alzheimer’s Disease CED Study Registry, facilitating the implementation of this coverage.
Eligibility Criteria and Market Potential: Leqembi is suitable for patients with mild cognitive impairment and mild dementia caused by Alzheimer’s disease, collectively called early-stage Alzheimer’s disease. Approximately 1.5 million people in the United States fall within this eligibility range. However, it is important to note that a larger population of approximately five million individuals has progressed beyond the scope of Leqembi’s eligibility. Consequently, an estimated 3% of Medicare beneficiaries may be eligible for this drug, which comes at an annual cost of $26,500.
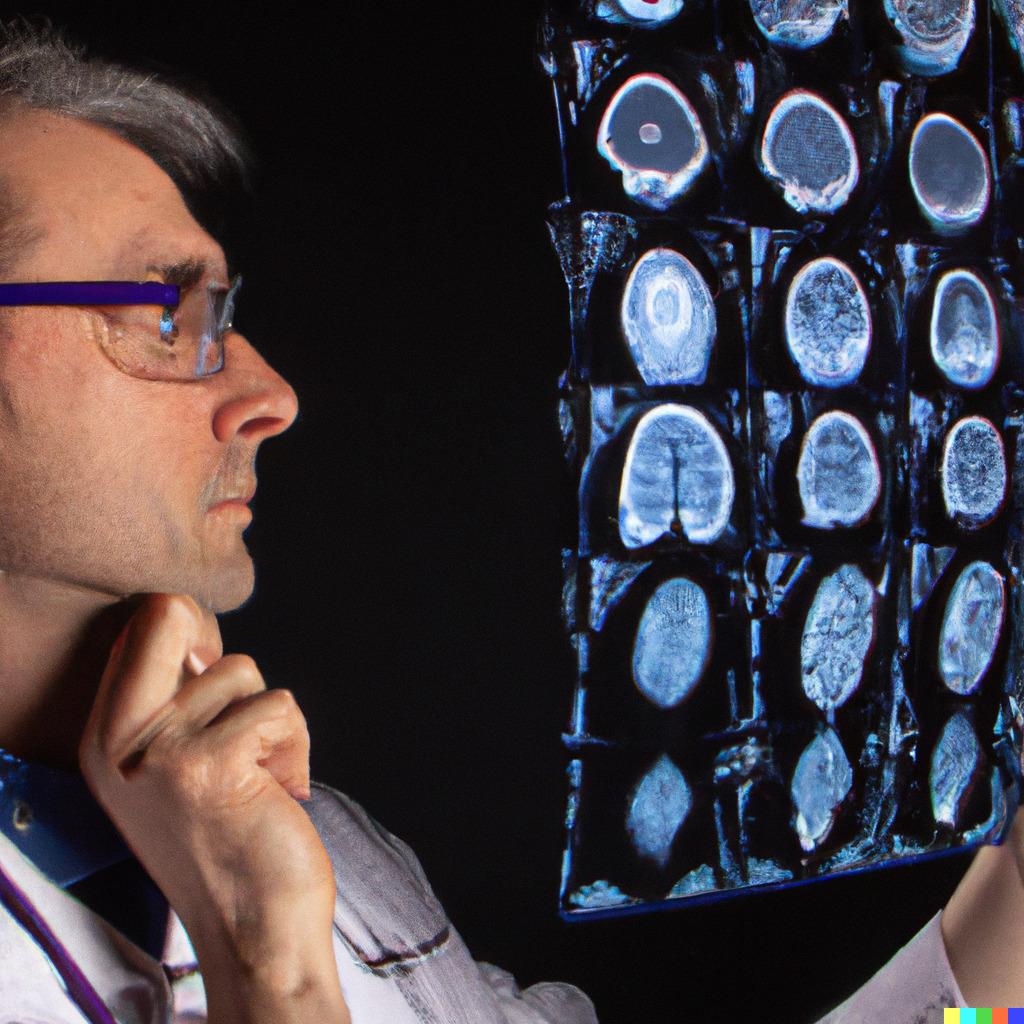
Significant Side Effects and Risk Considerations: Leqembi carries several notable black box warnings, with one of the most common side effects being ARIA (Amyloid related imaging abnormalities). Patients who are ApoE4 homozygous (carriers of two copies of the ApoE4 allele) likely face an increased risk of ARIA. Although ARIA is usually asymptomatic and occurs early in treatment, serious and life-threatening events such as edema and brain bleeds are rare but possible. Given these risks, prescribing Leqembi and similar anti-amyloid drugs should be limited to Alzheimer’s-experienced specialists, which in most cases is a Cognitive/Behavioral Neurologist. A comprehensive vetting process involving an MRI scan, confirmed beta-Amyloid pathology, and an ApoE4 status test should be followed (or at least strongly encouraged), with a thorough risk-benefit discussion with the patient.
Challenges in Supply and Patient Acceptance: Behavioral neurologists specializing in this field are in short supply, leading to extended waiting times of over 10 months. Additionally, both patients and healthcare professionals will require time to become acquainted with the medication and its protocols before widespread use can be expected. These factors, combined with the significant risks involved, may deter a considerable proportion of patients from pursuing Leqembi as a treatment option.
Cost Implications and Potential Savings: Considering all the aforementioned factors, it is projected that less than 1% of Medicare beneficiaries will seek access to Leqembi within the next year. As a result, the additional cost, including diagnostic workup expenses, is estimated to be less than $150 USD per year per average Medicare beneficiary.
However, it is essential to recognize the potential medical cost savings resulting from delaying cognitive decline. These savings are estimated to be up to $4,000 per member receiving the medication per year, translating to an average of $60 per Medicare member.
Furthermore, the introduction of disease-modifying therapy is expected to close coding gaps for dementia diagnosis, as currently 60% of cases go undiagnosed. The availability of Leqembi and the increased media attention surrounding it are likely to enhance willingness to undergo testing and receive a diagnosis. With a risk adjustment benefit of $3,000 to $5,000 per diagnosed member per year, even a modest 5% increase in diagnosis rates could result in a $20 revenue increase per member for Medicare Advantage plans.
Anticipated Coverage by Medicare Advantage Plans: While CMS has confirmed coverage for Leqembi, Medicare Advantage plans have yet to make significant announcements regarding its inclusion in their coverage. However, it is widely expected that they will follow CMS’s lead. To control the cost increase, it is crucial for Medicare Advantage plans and risk-bearing health systems to establish robust safeguards, step-up protocols, and prior authorization protocols. These measures will ensure that the drug is offered only to patients who stand to benefit significantly and have a favorable risk-benefit balance. Implementing such controls could potentially reduce the cost implication per average Medicare member to as low as $30 per year.
Partnering with Isaac Health for Effective Implementation: Isaac Health is committed to supporting health plans and health systems in implementing appropriate protocols and prior authorization processes. We understand the challenges and complexities surrounding the introduction of novel treatments such as Leqembi. If you are interested in our assistance, please schedule a time with our payer support team to explore commitment free how we can work together. The savings potential of getting protocols right is substantial.
Conclusion: The full approval of Leqembi marks a groundbreaking development in Alzheimer’s treatment. As health insurance employees, understanding the implications of this approval is vital for effective coverage decisions. By considering the eligibility criteria, potential cost implications, risk factors, and anticipated coverage by Medicare Advantage plans, health insurance payers can navigate the challenges associated with Leqembi’s introduction and ensure appropriate patient access to this significant disease-modifying therapy.
Please also see:
Our services for healthcare partners
Book a time for a conversation